High Attenuation pattern
Increased lung attenuation is called ground-glass-opacity (GGO) if there is a hazy increase in lung opacity without obscuration of underlying vessels and is called consolidation if the increase in lung opacity obscures the vessels.
In both ground glass and consolidation the increase in lung density is the result of replacement of air in the alveoli by fluid, cells or fibrosis.
In GGO the density of the intrabronchial air appears darker as the air in the surrounding alveoli.
This is called the 'dark bronchus' sign
In consolidation, there is exclusively air left intrabronchial.
This is called the 'air bronchogram'.
Ground-glass opacity
Ground-glass opacity (GGO)
represents:- Filling of the
alveolar spaces with pus, edema, hemorrhage, inflammation or tumor cells.
- Thickening of the
interstitium or alveolar walls below the spatial resolution of the HRCT as
seen in fibrosis.
The location of the abnormalities in ground glass pattern can be helpfull:
- Upper zone
predominance: Respiratory bronchiolitis, PCP.
- Lower zone
predominance: UIP, NSIP, DIP.
- Centrilobular
distribution: Hypersensitivity pneumonitis, Respiratory bronchiolitis
Thus ground glass in itself is very
unspecific.
Not suprisingly, there is a big overlap in the causes of ground-glass opacity and consolidation and some diseases may present with both areas of ground-glass and consolidation.
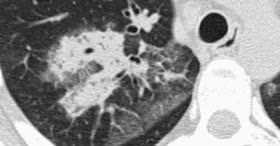
Here we see consolidation and ground-glass opacity in a patient with persistent
chest abnormalities and weight loss without signs of infection.Not suprisingly, there is a big overlap in the causes of ground-glass opacity and consolidation and some diseases may present with both areas of ground-glass and consolidation.
This suggested a chronic disease.
There is no honeycombing or traction bronchiectasis, so we can rule out fibrosis.
The weight loss is suggestive of a malignant disease.
Histology revealed broncho-alveolar cell carcinoma
Broncho-alveolar cell carcinoma
(BAC) may present as:
- solitary nodule or mass (40% of patients)
- focal or diffuse consolidation (30%) as in this case.
- diffuse ill-defined centrilobular nodules (30%) due to
endobronchial spread.
Treatable or not treatable?
Ground-glass opacity is nonspecific, but highly significant finding since 60-80% of patients with ground-glass opacity on HRCT have an active and potentially treatable lung disease.
In the other 20-40% of the cases the lung disease is not treatable and the ground-glass pattern is the result of fibrosis.
In those cases there are usually associated HRCT findings of fibrosis, such as traction bronchiectasis and honeycombing.
Ground-glass opacity is nonspecific, but highly significant finding since 60-80% of patients with ground-glass opacity on HRCT have an active and potentially treatable lung disease.
In the other 20-40% of the cases the lung disease is not treatable and the ground-glass pattern is the result of fibrosis.
In those cases there are usually associated HRCT findings of fibrosis, such as traction bronchiectasis and honeycombing.
Here are two cases with GGO, one without fibrosis and potentially treatable and the other with traction bronchiectasis indicating fibrosis.
Here is a CT with GGO as dominant pattern.
In addition there is traction bronchiectasis indicating the presence of fibrosis.
This case is one of the possible patterns of nonspecific interstitial pneumonia (NSIP).
NSIP is characterized histologically by a relatively uniform pattern of cellular interstitial inflammation associated with variable degrees of fibrosis.
As in UIP (usual interstitial pneumonia) it mainly involves the dependent regions of the lower lobes, but NSIP lacks the extensive fibrosis with honeycombing.
NSIP may be idiopathic or associated with collagen vascular diseases or exposure to drugs or chemicals.
NSIP has a relative good prognosis and the majority of patients respond to treatment with corticosteroids. This outcome is quite different from that seen in UIP, which has a poor prognosis.
Mosaic attenuation
The term 'mosaic attenuation' is
used to describe density differences between affected and non-affected lung
areas.There are patchy areas of black and white lung.
The role of the radiologist is to determine which part is abnormal: the black or the white lung.
When ground glass opacity presents as mosaic attenuation consider:
- Infiltrative
process adjacent to normal lung
- Normal lung
appearing relatively dense adjacent to lung with air-trapping
- Hyperperfused lung
adjacent to oligemic lung due to chronic thromboembolic disease
It can be difficult to distinguish
these three entities.
There are two diagnostic hints for
further differentiation:
- Look at expiratory scans for air trapping
- Look at the vessels
If the vesses are difficult to see
in the 'black' lung as compared to the 'white' lung, than it is likely that the
'black' lung is abnormal.
Then there are two possibilities: obstructive bronchiolitis or chronic pulmonary embolism.
Sometimes these can be differentiated with an expiratory scan.
If the vessels are the same in the 'black' lung and 'white' lung, then you are looking at a patient with infiltrative lung disease, like the one on the right with the pulmonary hemmorrhage.
Then there are two possibilities: obstructive bronchiolitis or chronic pulmonary embolism.
Sometimes these can be differentiated with an expiratory scan.
If the vessels are the same in the 'black' lung and 'white' lung, then you are looking at a patient with infiltrative lung disease, like the one on the right with the pulmonary hemmorrhage.
Temporary bronchiolitis with air
trapping is seen in:
- (post) infection
- Inhalation of toxin
- Rheumatoid arthritis, Sj?gren
- Post transplant
- Drug reaction (penicillamine)
HRCT
of a patient with ground glass pattern in a mosaic distribution.
Some lobules are involved and others are not.
The differential diagnosis is hypersensitivity pneumonitis, bronchiolitis or thromboembolic disease.
The history was typical for hypersensitivity pneumonitis.
Hypersensitivity pneumonitis usually presents with centrilobular nodules of ground glass density (acinar nodules).
When they are confluent, HRCT shows diffuse ground glass.
·
Hypersensitivity
pneumonitis (HP) is an allergic lung disease caused by the
inhalation of antigens contained in a variety of organic dusts.
Farmer's lung is the best-known HP syndrome and results from the inhalation of fungal organisms that grow in moist hay or exposure to birds as pets .
HP usually presents in two forms either as ground glass in a mosaic distribution as in this case or as centrilobular nodules of ground glass density (acinar nodules).
Farmer's lung is the best-known HP syndrome and results from the inhalation of fungal organisms that grow in moist hay or exposure to birds as pets .
HP usually presents in two forms either as ground glass in a mosaic distribution as in this case or as centrilobular nodules of ground glass density (acinar nodules).
Above is a patient with ground glass
pattern in a mosaic distribution.
The clue here is the enlargement of pulmonary arteries (arrow) in the areas of ground glass.
The ground glass appearance is the result of hyperperfused lung adjacent to oligemic lung with reduced vessel caliber due to chronic thromboembolic disease.
The clue here is the enlargement of pulmonary arteries (arrow) in the areas of ground glass.
The ground glass appearance is the result of hyperperfused lung adjacent to oligemic lung with reduced vessel caliber due to chronic thromboembolic disease.
CT of another patient with ground glass
pattern in a mosaic distribution.
Again the ground glass appearance is the result of hyperperfused lung with large vessels adjacent to oligemic lung with small vessels due to chronic thromboembolic disease.
Emboli adherent to the wall and intravascular septa are typical for chronic thromboemboli in which partial recanalization took place.
Again the ground glass appearance is the result of hyperperfused lung with large vessels adjacent to oligemic lung with small vessels due to chronic thromboembolic disease.
Emboli adherent to the wall and intravascular septa are typical for chronic thromboemboli in which partial recanalization took place.
Crazy Paving
Crazy Paving is a combination of
ground glass opacity with superimposed septal thickening (5).It was first thought to be specific for alveolar proteinosis, but later was also seen in other diseases.
Crazy Pavin can also be seen in:
- Alveolar
proteinosis
- Sarcoid
- NSIP
- Organizing pneumonia
(COP/BOOP)
- Infection (PCP,
viral, Mycoplasma, bacterial)
- Neoplasm
(Bronchoalveolarca (BAC)
- Pulmonary
hemorrhage
- Edema (heart
failure, ARDS, AIP)
Consolidation
Consolidation is synonymous with
airspace disease.When you think of the causes of consolidation, think of 'what is replacing the air in the alveoli'?
Is it pus, edema, blood or tumor cells (Table above).
Even fibrosis as in UIP, NSIP and long standing sarcoidosis can replace the air in the alveoli and cause consolidation.
Acute consolidation is seen in:
- Pneumonias (bacterial, mycoplasma, PCP)
- Pulmonary edema due to heart failure or ARDS
- Hemorrhage
- Acute eosinophilic pneumonia
Chronic consolidation is seen in:
- Organizing Pneumonia
- Chronic eosinophilic pneumonia
- Fibrosis in UIP and NSIP
- Bronchoalveolar carcinoma or lymphoma
Most patients who are evaluated with
HRCT, will have chronic consolidation, which limits the differential diagnosis.
Here are two cases with chronic consolidation.
There are patchy non-segmental consolidations in a subpleural and peripheral distribution.
The differential diagnosis is the same as the list above.
The final diagnosis was cryptogenic organizing pneumonia (COP).
In chronic eosinophilic pneumonia the HRCT findings will be the same, but there will be eosinophilia.
In fibrosis there will be other signs of fibrosis like honeycombing or traction bronchiectasis.
Bronchoalveolar carcinoma can also look like this.
Organizing pneumonia (OP)
Organizing pneumonia represents an inflammatory process in which the healing process is characterized by organization and cicatrization of the exudate rather than by resolution and resorption.
It is also described as 'unresolved pneumonia'.
If no cause can be identified it is called cryptogenic organizing pneumonia (COP).
It was described in earlier years as Bronchiolitis-obliterans-organizing pneumonia (BOOP).
Patients with COP typically present with a several-month history of nonproductive cough.
Many cases are idiopathic, but OP may also be seen in patients with pulmonary infection, drug reactions, collagen vascular disease, Wegener's granulomatosis and after toxic-fume inhalation.
Seen here is a case of chronic eosinophilic pneumonia.
It was a patient with low-grade fever, progressive shortness of breath and an abnormal chest radiograph.
There was a marked eosinophilia in the peripheral blood.
Like in COP we see patchy non-segmental consolidations in a subpleural distribution.
Chronic eosinophilic pneumonia is an idiopathic condition characterized by extensive filling of alveoli by an infiltrate consisting primarily of eosinophils.
Chronic eosinophilic pneumonia is usually associated with an increased number of eosinophils in the peripheral blood and patients respond promptly to treatment with steroids.
ALSO READ THE OLDER POSTS














No comments:
Post a Comment
Please leave your comments